Arthropathy is the most common of all diseases of the musculoskeletal system. Inflammatory and non-inflammatory diseases can significantly deteriorate human quality of life and, in many cases, lead to disability. One of the most common diseases is knee osteoarthritis. Pathological symptoms are usually more severe and require qualified assistance.
cause of disease
In medical terms, the disease is also known as osteoarthritis, knee disease, deforming osteoarthritis (DOA). Arthropathy is a collective term for all degenerative dystrophic diseases of the joints and intervertebral joints. Violations of the knee area are called knee arthropathy.

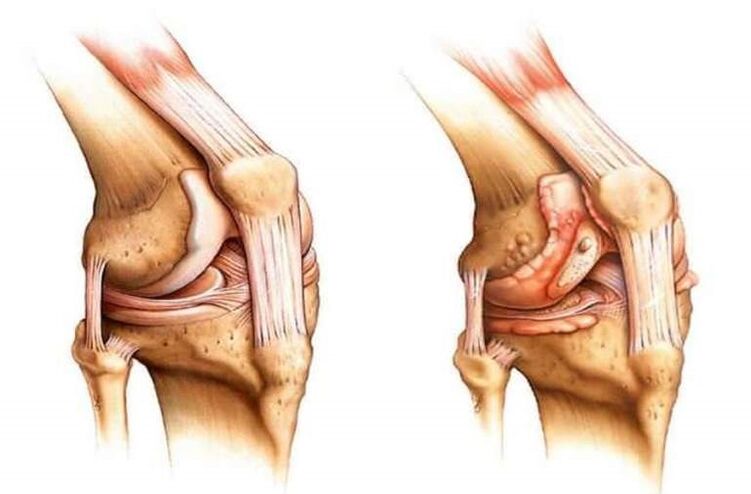
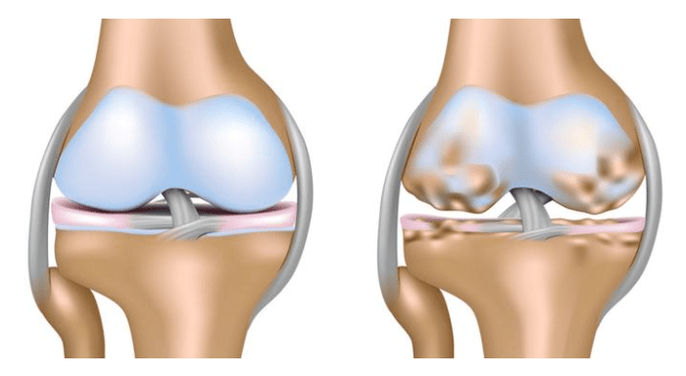
It is characterized by damaged knee cartilage.
Pathology includes degenerative dystrophic changes in bone and cartilage tissue characterized by progressive thinning of cartilage and parallel formation of bone growths in articular joints.
This becomes the body's response to increased friction and stress. The most likely causes of knee arthropathy symptoms are as follows:

- Mild and severe trauma with long-term impairment of joint mobility. Ruptured or severely bruised ligaments often trigger an inflammatory process that triggers the symptoms of arthropathy.
- Surgical intervention on the knee joint to remove any defects or foreign bodies.
- Sustained prolonged and excessive physical activity. This could be due to professional sports or professions. Continued tension in the connecting area can lead to progressive thinning of the cartilage, which can negatively affect the entire musculoskeletal system.
- Acute bursitis is accompanied by the development of purulent inflammation of the joint cavity. Often, it is difficult to get rid of this pathology in a conservative manner, so doctors resort to minor surgical interventions, which can adversely affect cartilage tissue.
- Arthritis of all forms and severity. In this case, the inflammatory process is evident, proceeds with a sharp increase in temperature and leads to the development of arthropathy after some time.
- Gout also frequently results in cartilage lesions with severe clinical manifestations and joint deformities.
- Immunity is weakened and bone and cartilage tissue gradually regresses as the body is unable to cope with the pathology.
- Bad habits - alcoholism, smoking - are often predisposing factors for the development of pathological signs.
- Severe autoimmune disease.
- Frequent viral and catarrhal lesions induce the development of inflammatory processes and degenerative dystrophic changes.
- Overweight and severe obesity can also lead to violations, because every kilogram added increases the load on the joints by a factor of 10, which definitely affects the cartilage tissue.
It's worth noting that all of these reasons most often trigger minor types of violations. There is also a major difference in that the disease becomes the result of the body's natural aging process. Bone and cartilage tissue wears down, which increases friction and pressure. The result is knee arthropathy.
various pathologies
There are several types of pathological conditions, each with its own characteristics. Depending on how the joints are affected, the following types of disorders can be distinguished:
- The right side is characterized by changes in the right cartilage tissue. Often, it becomes the initial stage of the disease.
- Depending on the nature of the clinical presentation, the signs of knee arthropathy on the left side were indistinguishable from those on the right side. But it's worth noting that this type often occurs in overweight patients.
- Bilateral refers to the severe form, affecting the entire cartilage and characterized by severe pain.
Notably, the latter type is more common in older patients with primary tissue damage. According to the course of the pathological process, acute and chronic types are distinguished. The first is characterized by rapid progression and the development of complications, and the second is slow and may not bother the patient for several years.
clinical picture
The signs of knee arthropathy and its symptoms largely depend on the degree of damage to the joint. Currently, the pathological process has several stages, each with its own clinical manifestations:

- The initial stage is characterized by the absence of overt symptoms and the inability to visually identify the pathology. The patient was more tired than usual, but recorded it as overexertion or increased workload. He became lethargic, lethargic, and his performance plummeted. Some patients experience mild joint stiffness with activity, especially in the morning. However, they usually don't pay attention to this and don't turn to experts. If the joint is X-rayed at this stage, a narrowing of the joint space can be noticed, which can trigger a violation.
- In the next stage, the discomfort and stiffness will not go away, but only increase. Under light and brief loads, patients experience severe knee pain that disappears only with prolonged rest. In some cases, the joints are swollen, which goes away at night but reappears during the day. As the pressure on cartilage tissue increases due to its depletion, patients often hear a characteristic creaking sound during exercise. Flexion function is also impaired because the patient cannot fully flex the limb. At this stage, patients usually turn to specialists.
- The third stage is the most severe and is characterized by a pronounced pain syndrome in patients not only during exercise but also at rest. In severe cases, the pain does not leave a person even at night, which can significantly worsen his condition. Puffiness at this stage is constantly observed. In the joint pocket, the amount of synovial fluid is drastically reduced, which increases the load and increases the friction of the joint.
- The initial stage is characterized by the absence of overt symptoms and the inability to visually identify the pathology. The patient was more tired than usual, but recorded it as overexertion or increased workload. He became lethargic, lethargic, and his performance plummeted. Some patients experience mild joint stiffness with activity, especially in the morning. However, they usually don't pay attention to this and don't turn to experts. If the joint is X-rayed at this stage, a narrowing of the joint space can be noticed, which can trigger a violation.
- In the next stage, the discomfort and stiffness will not go away, but only increase. Under light and brief loads, patients experience severe knee pain that disappears only with prolonged rest. In some cases, the joints are swollen, which goes away at night but reappears during the day. As the pressure on cartilage tissue increases due to its depletion, patients often hear a characteristic creaking sound during exercise. Flexion function is also impaired because the patient cannot fully flex the limb. At this stage, patients usually turn to specialists.
- The third stage is the most severe and is characterized by a pronounced pain syndrome in patients not only during exercise but also at rest. In severe cases, the pain does not leave a person even at night, which can significantly worsen his condition. Puffiness at this stage is constantly observed. In the joint pocket, the amount of synovial fluid is drastically reduced, which increases the load and increases the friction of the joint.

Often, the pain disrupts the patient's sleep, and he becomes irritable and constantly fatigued. Decreased or completely absent appetite, leading to a deterioration in the work of the digestive and cardiovascular systems.
Lack of normal sleep often leads to neurasthenia, especially in elderly patients or young adults with high-intensity physical labor. Memory impairment and inattention are also a result of the patient's lack of rest.
Usually, the pathology proceeds in the absence of temperature, but in advanced stages, when the cartilage is completely destroyed, the friction of the bones and the pressure between them increases, triggering an inflammatory process.
The body tries to restore balance and reduce the load on the connection. It is for this reason that osteophytes, or bone growths, develop in joints. They become the cause of late deformation of the pathological process.
The most dangerous complication of such violations would be complete immobilization and disability of the patient. Often, this occurs without proper treatment or long-term neglect of knee osteoarthritis symptoms.
diagnosis method
For an accurate diagnosis, doctors recommend that patients undergo a thorough examination. This is not only necessary to determine the cause, but also for the correct selection of the drugs needed for treatment. The first step will be to interview the patient and identify possible causes. Lifestyle, occupational activities and habits play a special role. The next step will be to examine the affected limb and determine the extent of the damage.

If there are no obvious signs of pathology, the disease is in an early stage. The next step will be to take a medical history and identify chronic conditions that may be precipitating factors. Afterwards, patients donated blood for laboratory testing. Traces of inflammation in it, detected in the form of elevated levels of white blood cells, suggest that some process contributes to the development of the disease.
A mandatory moment in the diagnosis will be an X-ray to accurately determine the extent of the arthropathy. Pictures usually show areas of complete cartilage destruction, as well as the number and location of osteophytes. This helps clarify the presumptive diagnosis and prescribe appropriate treatment.
It is sometimes impossible to see the exact picture and extent of damage to the joint on an X-ray. In this case, an ultrasound examination of the joint is recommended.
In extreme cases, patients are asked to have a CT scan. This is usually enough to get a full picture of the disease.
medical treatement
Conservative treatment of pathological conditions is only possible in stages 1 and 2, when osteophyte formation has not yet begun. The main goal of treatment is to slow the destruction and recovery of cartilage. The classic regimen involves the use of the following drugs:
- From the group of pain relievers that help relieve pain. Makes patients feel better and improves nighttime sleep. In the hospital, injections are effective and given 1 to 3 times a day under the supervision of a specialist. Long-term use of funds is not recommended, as they do not affect the progression of the pathological process, but only relieve acute pain.
- Non-steroidal anti-inflammatory drugs. Funding, available in tablet and injection forms, not only eliminates acute pain, but also slows pathological progression, relieves localized heat and swelling, and improves motor function. With regular intake for 7-10 days, a constant concentration of the active ingredient of the drug is observed in the patient's blood, thus ensuring a prolonged action. Taking medications for extended periods of time is not recommended because they often have adverse effects on the digestive system. Therefore, patients with severe peptic ulcers or other medical conditions should not take them.
- Chondroprotective agents help restore cartilage in affected joints and increase synovial fluid volume. Typically, such medications contain glucosamine and chondroitin. Long-term use is recommended. Typically, 8-12 week courses are prescribed, with regular visits to specialists to spot improvements. Clear instructions can extend reception time.
- Glucocorticoids. They are used to treat advanced cases when the pain syndrome cannot be eliminated by conventional methods. Helps reduce swelling and pain. It is only allowed to be administered intramuscularly or intravenously in hospitals.
- Non-steroidal anti-inflammatory drugs. Funding, available in tablet and injection forms, not only eliminates acute pain, but also slows pathological progression, relieves localized heat and swelling, and improves motor function. With regular intake for 7-10 days, a constant concentration of the active ingredient of the drug is observed in the patient's blood, thus ensuring a prolonged action. Taking medications for extended periods of time is not recommended because they often have adverse effects on the digestive system. Therefore, patients with severe peptic ulcers or other medical conditions should not take them.
- Chondroprotective agents help restore cartilage in affected joints and increase synovial fluid volume. Typically, such medications contain glucosamine and chondroitin. Long-term use is recommended. Typically, 8-12 week courses are prescribed, with regular visits to specialists to spot improvements. Clear instructions can extend reception time.
- Glucocorticoids. They are used to treat advanced cases when the pain syndrome cannot be eliminated by conventional methods. Helps reduce swelling and pain. It is only allowed to be administered intramuscularly or intravenously in hospitals.
In addition to these funds, patients are prescribed courses of external medication in the form of ointments, creams or gels. The latter option is the most preferred because of its rapid penetration into the joint cavity and therapeutic effect. They can be used within 14 days. Extending the course on your own is not recommended because of the increased risk of complications.
In the most severe cases, the patient is injected directly into the joint cavity. You can use traditional pain relievers, but the best therapeutic effect is achieved by introducing hyaluronic acid preparations. 1 injection over 7 days. For complete pain relief, 3-5 injections are sufficient. After such treatment, the effect lasts for 6 months. The patient has normal mobility and the pain syndrome has almost completely disappeared.
If none of these approaches have the desired effect, and the patient's condition deteriorates, surgery is performed to replace the joint with a prosthesis. Replace the entire joint or its individual parts. This usually applies to arthropathy caused by severe knee injuries. The surgery is performed under general anesthesia, and the recovery period is quite long and difficult.
Knee arthropathy is a severe degenerative dystrophic pathology that, if not treated properly, can lead to disability in patients. It is recommended that you consult a doctor immediately at the first signs of a violation.














































